Your Body's Story: Releasing Trauma Through Movement and Somatics
Why Your Body Remembers What Your Mind Forgets

Have you ever felt a knot in your stomach when entering a certain room, or found your shoulders tensed up to your ears without knowing why? This is your body speaking a language older than words. Learning how to physically release trauma from the body begins with honoring a fundamental truth: trauma is not just a memory or a story you tell; it is a profound physical experience etched into your very being. When we encounter overwhelming events—whether a single incident or a prolonged period of distress—our nervous system shifts into survival mode. It floods our body with energy to fight, flee, or freeze. If that intense survival energy isn't fully discharged and resolved, it can remain stored in our muscles, fascia, and tissues. This trapped energy can manifest as chronic tension, persistent anxiety, digestive issues, or a pervasive feeling of being disconnected from yourself and the world.
Your body holds the complete story of your experiences, but it also holds the innate wisdom and capacity for healing. The same nervous system that stored the trauma has an inherent ability to release it and return to a state of balance. This healing process can be profoundly supported through personalized, body-aware care that honors your unique pace, history, and needs. My approach integrates several key elements:
- Attachment-Focused EMDR: An evidence-based therapeutic model that helps your brain and body reprocess and integrate stuck memories, sensations, and emotions. It uses bilateral stimulation (like guided eye movements) while prioritizing the foundational elements of safety, choice, and a secure therapeutic connection.
- EMDR Intensives (when appropriate): A time-condensed format designed for focused, goal-oriented work. This can support deeper, more concentrated processing for individuals who are ready for it.
- Nervous-System Regulation Skills: Gentle, practical, and accessible tools—such as grounding exercises and paced breathing—to help your body feel settled and safe, both between and during therapy sessions.
- One-on-One Professional Support: Working directly with a dedicated solo therapist ensures a highly personalized plan that adapts to your needs, rather than a generic, one-size-fits-all program.
As a Licensed Clinical Social Worker and Certified EMDR Therapist, I specialize in helping adults use personalized, attachment-focused EMDR and EMDR Intensives to facilitate this deep, body-based healing. My solo practice is dedicated to helping you access your body's natural wisdom to create lasting, meaningful change.
Understanding How Trauma Lives in Your Body
Your body's response to danger is an automatic, brilliant survival mechanism. The autonomic nervous system (ANS) acts like a highly sensitive smoke alarm, instantly triggering the fight, flight, or freeze response to protect you from perceived threats. This ancient system is incredibly effective. In a typical stress cycle, once the danger passes, your nervous system is designed to return to a calm, balanced, and socially engaged state (known as the ventral vagal state). This is where you feel safe, connected, and at ease.
However, during a traumatic event, this natural cycle can be violently interrupted. The immense surge of survival energy created to fight or flee doesn't get fully discharged, especially if the response was to freeze or shut down. This leaves your nervous system stuck in a state of high alert, unable to receive the "all-clear" signal. You might find yourself oscillating between hypervigilance, anxiety, and irritability (a sympathetic "fight-or-flight" state) or feeling numb, disconnected, exhausted, and hopeless (a parasympathetic "freeze" or shutdown state). This trapped energy essentially convinces your body that the threat is still present, even when you are logically and physically safe.
This chronic state of activation, or dysregulation, has profound and far-reaching effects. Scientific research shows that long-term stress and trauma impact nearly every system in your body, from your immune function and hormonal balance to your cardiovascular health. Recognizing that trauma is a physiological experience, not a personal failing, is the first and most crucial step toward healing. I explore this concept further in my article about where trauma is stored in the body.
Common Physical Manifestations of Stored Trauma
When trauma remains stuck, your body communicates its distress through a variety of physical symptoms. These are not "all in your head"; they are real, tangible signals that your nervous system is overburdened and deserves compassionate attention.
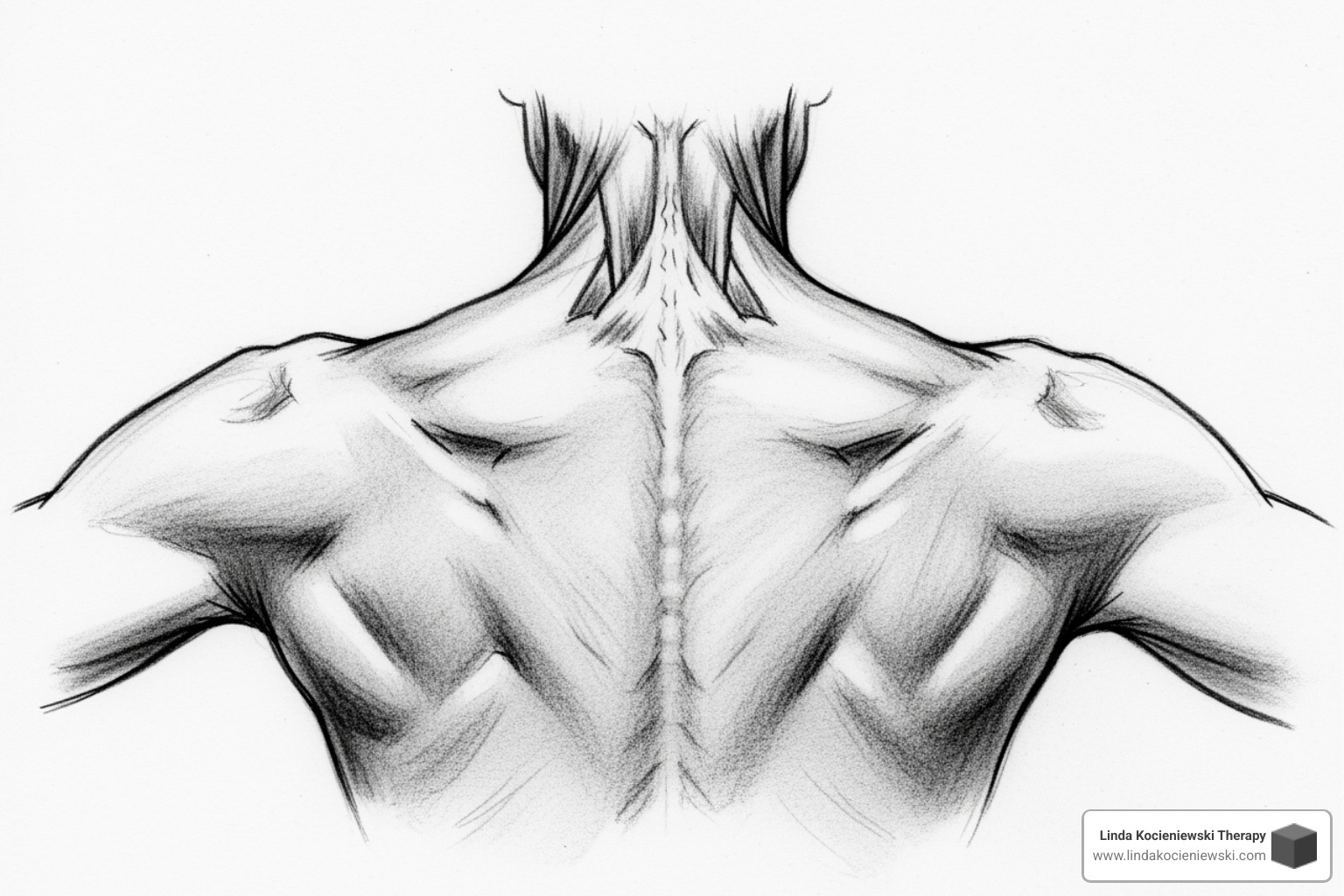
- Chronic Muscle Tension: Often called "body armoring," this is when your muscles brace for an anticipated danger and then forget how to let go. This tension commonly accumulates in the jaw (bruxism), shoulders, neck, back, and hips.
- Unexplained Pain and Aches: You may experience persistent pain, stiffness, or conditions like fibromyalgia that have no clear medical cause. This is your body expressing held stress and unprocessed emotional pain physically.
- Headaches and Migraines: Constant tension in the muscles of the head, neck, face, and shoulders can restrict blood flow and trigger frequent, severe headaches or migraines.
- Digestive Issues: The gut is intricately linked to the brain via the gut-brain axis and is highly sensitive to stress. Stored trauma can lead to chronic issues like Irritable Bowel Syndrome (IBS), acid reflux, constipation, or chronic stomach upset.
- Fatigue and Sleep Disturbances: Being in a constant state of high alert (sympathetic) or shutdown (dorsal vagal) is physically and mentally exhausting. This can lead to chronic fatigue, adrenal exhaustion, insomnia, frequent waking, or nightmares.
- Shallow Breathing: A stressed nervous system defaults to rapid, shallow breathing in the upper chest. This pattern perpetuates the stress cycle by signaling to your brain that danger is present, preventing your system from settling.
Learning to listen to these signals with curiosity instead of judgment is the first step in understanding how to physically release trauma from the body.
How Attachment-Focused EMDR Supports Physical Release
When talking about a difficult experience isn't enough to create lasting change, it's often because the trauma is held in the non-verbal, sensory parts of the brain and body. Attachment-focused EMDR offers a powerful way to help your body and brain process what feels stuck on a physiological level. EMDR (Eye Movement Desensitization and Reprocessing) uses bilateral stimulation (such as guided eye movements, alternating sounds, or gentle taps) to activate the nervous system's innate information processing system. This helps the brain integrate fragmented memories, sensations, beliefs, and emotions associated with the trauma.
In an attachment-focused approach, we prioritize creating a safe and trusting therapeutic relationship. We go at a pace that keeps your nervous system within a tolerable range of emotion (your "window of tolerance"), emphasizing safety, choice, and connection every step of the way. This is a dual top-down and bottom-up process. The "top-down" aspect involves the cognitive insights and new perspectives you gain, while the "bottom-up" aspect is the direct processing and release of sensations and emotions from the body. As your brain reprocesses overwhelming experiences, the body often follows suit—chronic muscular bracing can soften, breathing naturally deepens, and the constant hum of the stress response begins to quiet. Many adults who engage in EMDR report significant improvements like better sleep, fewer emotional triggers, and a marked decrease in physical tension as their system finally learns it no longer needs to stay on high alert.
How to Physically Release Trauma From the Body with Simple, Grounding Practices
While deeper trauma processing is best guided by a trained therapist, you can support your body between sessions with gentle regulation practices. The most important principle is to cultivate a sense of safety and self-regulation. If any practice feels too intense or activating, pause, and return to what feels steady and present. These are invitations, not commands.

- Grounding Through the Senses: This practice anchors you in the present moment. Gently press your feet into the floor. Notice the texture of the ground beneath you. Feel the solid support of your chair against your back and legs. Let your eyes gently scan the room and find three things that signal "safe" or "neutral" to you, noticing their color, shape, and texture.
- Paced Breathing (Vagal Toning): Inhale slowly through your nose for a count of 4, hold gently for a moment, and then exhale slowly through pursed lips for a count of 6 or 8. The longer exhale is key, as it stimulates the vagus nerve, which acts as a brake for your body's stress response. Repeat this for 2–3 minutes, allowing your body to settle with each breath.
- Hand-to-Heart Support: Rest one hand over the center of your chest and one over your belly. Simply feel the warmth of your hands and the gentle rise and fall of your breath beneath them. This simple act can release oxytocin, a hormone associated with safety and connection. If it feels right, add a quiet, compassionate phrase like, "I'm here; I'm safe enough in this moment."
These practices are not meant to force a release but to create the safe internal conditions for your body's natural healing intelligence to emerge when it's ready.
Deepening the Work with Attachment-Focused EMDR and EMDR Intensives
While there are many valuable modalities for body-based healing, my approach centers on attachment-focused EMDR. This method is specifically adapted to honor your relational history, your nervous system's pace, and your personal goals. Unlike some therapies that might push you into distressing material too quickly, we begin by building resources. This involves co-creating a toolkit of internal anchors—skills, memories of strength, and imagined safe places—that help you feel steadier and more capable of navigating difficult emotions. Only then do we approach the challenging material. From there, EMDR uses bilateral stimulation to help your brain reprocess and reconsolidate stuck memories, allowing your body to finally understand that the danger is over and it no longer needs to brace for impact.
This approach is defined by several key principles:
- Personalized and Paced: We work in manageable, digestible pieces, a process known as titration. This ensures your system stays within your window of tolerance, preventing re-traumatization and making the process feel safe and effective.
- Relational and Attachment-Focused: The therapeutic relationship itself becomes a healing agent. It provides a secure, reliable container for exploring what was overwhelming in the past, at a pace that feels right for you. For more information on the standards and practice of EMDR, you can visit the EMDR International Association (EMDRIA).
- Body-Aware: Healing happens in the present moment. As processing unfolds, we continuously track the shifts in your breath, posture, physical sensations, and emotions. Your body’s signals become a primary guide for the work.
EMDR Intensives: When a Focused Format Helps
For some adults, a time-condensed EMDR Intensive offers a supportive and powerful way to focus more deeply on a specific goal without the weekly interruption of traditional therapy. An intensive format allows for extended sessions over several days, which can facilitate deeper processing and integration by minimizing the time spent opening and closing a topic each week. Intensives are not a one-size-fits-all solution; we decide together if this format is a good fit for your needs based on your history, current stability, capacity for self-regulation, and desired outcomes. If it’s appropriate, we’ll create a personalized plan that includes thorough preparation, targeted reprocessing of specific memories or themes, and robust integration strategies so you leave with clarity, relief, and ongoing support.
The Role of EMDR in Releasing the Body’s Stress Response
Traumatic memories are often not stored like regular memories; they are fragmented and frozen in the nervous system, complete with the original sensory data, emotions, and physical sensations. This is why a certain smell or sound can trigger a full-body reaction as if the danger is happening right now. EMDR engages bilateral stimulation to help the brain's information processing system access and reprocess these stuck memories. As this happens, the physical and emotional charge of the memories can diminish significantly. Many people report feeling physically lighter, as if a heavy weight has been lifted, as chronic tension, hypervigilance, and other somatic symptoms begin to relax and resolve. You can learn more about this process in my article on Trauma and EMDR.
Recognizing the Signs and Supporting the Process of Release
As you learn how to physically release trauma from the body, it's incredibly helpful to recognize the signs that your nervous system is processing and discharging stored energy. The experience is unique to each person and can be subtle or pronounced, but common signs often fall into three categories:
- Physical Signs: These are direct manifestations of the nervous system shifting gears. You might experience involuntary shaking, trembling, or twitching (known as neurogenic tremors), which is the body's natural way of releasing pent-up fight-or-flight energy. Other signs include tingling sensations, waves of warmth or coolness spreading through the body, deep yawning, sighing, or spontaneous tears that feel cleansing rather than sad.
- Emotional Signs: As stored energy moves, so do the emotions attached to it. You might experience sudden waves of sadness, anger, or fear that surface and then pass, often followed by a sense of relief, calm, or lightness. Spontaneous moments of joy, deep peace, or a feeling of profound connection can also emerge as the nervous system returns to a more regulated state.
- Cognitive Signs: Release isn't just physical; it changes how you think. You may have new insights about old patterns, a sudden understanding of why you've behaved in certain ways, or memories surfacing without their usual emotional charge. These are often described as "aha moments" that bring clarity and a new perspective on your past.
These are all positive signs of your body's natural intelligence at work, completing biological processes that were interrupted long ago. You can learn more about the signs your body is releasing trauma to better understand and support your healing journey.
How to Physically Release Trauma From the Body by Creating a Safe Space
Creating a palpable sense of safety is the single most critical component of this work. Your nervous system will only allow the release of long-held tension when it genuinely perceives safety in the present moment. This involves cultivating both internal safety (your relationship with yourself) and external safety (your environment and relationships).

- Use Grounding Techniques: When sensations or emotions feel intense, grounding techniques anchor you in the here and now. The 5-4-3-2-1 technique is excellent for this: gently notice 5 things you can see, 4 things you can physically feel (your feet on the floor, the fabric of your shirt), 3 things you can hear, 2 things you can smell, and 1 thing you can taste. This pulls your attention out of past-based fear and into present-moment reality.
- Practice Radical Self-Compassion: Healing is not a linear process and it takes time. Treat yourself with the same kindness, patience, and understanding you would offer a dear friend who is suffering. Research on self-compassion shows it actively supports the neurobiological changes needed for trauma recovery by calming the threat response.
- Journal Your Experience: Create a dialogue between your mind and body by tracking your experiences. Note physical sensations, feelings, and insights without judgment. You might ask yourself: "Where do I feel this in my body?" "What does this sensation need?" This practice helps you recognize progress and honor your body's messages.
- Create Gentle, Predictable Routines: Consistency signals safety to your nervous system. A few minutes of deep breathing each morning, a short body scan before bed, or a gentle stretching routine can create a predictable rhythm that feels supportive and calming, not stressful or demanding.
This work is never about forcing a release, but about patiently and compassionately creating the conditions for your body's natural healing intelligence to emerge.
The Importance of Professional Guidance in Trauma Recovery
While self-help practices are valuable and empowering for managing daily stress, learning how to physically release trauma from the body, especially complex or deep-seated trauma, is best undertaken with professional support. Navigating the powerful currents of stored survival energy alone can sometimes feel overwhelming, disorienting, or even re-traumatizing if not handled with skill and care.
As a solo trauma therapist, I provide a safe, steady, and knowledgeable "container" for your healing. My role is to help you steer overwhelming emotions safely, ensuring that the release process happens at a pace your nervous system can integrate. This involves two key therapeutic concepts: titration, where we touch on distressing material in small, manageable doses, and pendulation, where we guide you in gently moving between the difficult sensation and a place of resource or ease in your body. This prevents your system from becoming flooded. This is where co-regulation becomes vital. My calm, attuned, and regulated presence supports your nervous system in feeling safe enough to relax and let go, modeling a state of balance that you can eventually learn to cultivate on your own.
For complex trauma, which often stems from repeated or prolonged difficult experiences (especially during childhood), specialized care is essential. These patterns of survival become deeply embedded in the nervous system, personality structure, and sense of self. In these cases, the therapeutic alliance—the trusting, collaborative relationship between you and me—becomes a powerful healing force in itself. It provides a foundation of relational safety and trust that may have been missing in the past, allowing for the repair of attachment wounds alongside the processing of traumatic events.
How I Guide Your Process
As a Licensed Clinical Social Worker and Certified EMDR Therapist, I understand that true healing must involve both mind and body. My commitment is to guide you with expertise and compassion. I will help you:
- Create a personalized healing plan that is custom-fit to your specific history, goals, nervous system capacity, and life circumstances, using attachment-focused EMDR and, when appropriate, EMDR Intensives.
- Integrate physical release with psychological processing by skillfully tracking sensations, emotions, images, and thoughts as they shift during EMDR, ensuring the work feels coherent, grounded, and meaningful.
- Stay within your "window of tolerance" by carefully pacing sessions, teaching you practical regulation skills you can use in daily life, and ensuring you always have a clear path back to feeling settled and centered.
This professional partnership allows your body's innate wisdom to guide the healing process within a framework of skillful, compassionate, one-on-one support.
Frequently Asked Questions about Physically Releasing Trauma
As you explore the profound topic of how to physically release trauma from the body, it's natural and wise to have questions. Here are answers to some of the most common inquiries I receive from clients.
Is it safe to release trauma on my own?
This is a crucial question with a nuanced answer. For general stress, accumulated tension from a tough week, or mild emotional upset, gentle self-guided practices like deep breathing, mindful stretching, or yoga are generally safe and highly beneficial. However, when addressing deep-seated, developmental, or complex trauma, professional guidance is not just recommended—it is essential for safety. Attempting to release significant trauma alone can risk overwhelming your nervous system, leading to feelings of fragmentation, destabilization, or re-traumatization. A trained therapist provides a safe, contained space and acts as a co-regulator for your nervous system, ensuring the process is healing rather than harmful. Think of it as having an expert guide for a challenging mountain trek; their presence and knowledge ensure you steer the terrain safely and effectively.
How long does it take to feel better?
There is no universal timeline for healing from trauma. The process is highly personal, non-linear, and unique to each individual's history and nervous system. Some people feel immediate shifts after beginning therapy, such as better sleep, a calmer baseline, or less muscle tension. For others, progress is more gradual and subtle. The most helpful approach is to release the pressure of a deadline and instead focus on consistent practice and radical self-compassion. Healing often happens in waves, with periods of intense processing and release followed by quieter periods of integration. These quieter times are not setbacks; they are an essential part of your nervous system reorganizing and adjusting to a new, healthier, and more regulated way of being.
What if I don't feel anything during these exercises?
This is completely normal and does not mean the exercises aren't working or that you are doing something wrong. If you have a history of trauma, your body likely developed intelligent protective systems, such as numbing or disconnecting (dissociation), as a brilliant survival strategy. The body will only release stored tension when it feels genuinely and deeply safe to do so. Building that profound sense of internal safety takes time and patience. Not feeling much at first can be your body's way of cautiously testing the waters. The key is to remain patient, curious, and consistent. By continuing to show up for yourself with gentle awareness and without judgment, you are sending a powerful new message to your nervous system: that it is finally safe to feel and to let go. Subtle shifts in your baseline state often precede more noticeable releases.
What's the difference between releasing trauma and simple relaxation?
This is an excellent question. While both are valuable, they are distinct processes. Relaxation aims to calm the nervous system and reduce current stress, often by engaging the parasympathetic nervous system (e.g., through meditation or a warm bath). It's about finding a state of ease in the present. Trauma release, on the other hand, is an active process of discharging stored survival energy from past events. This process can sometimes be energizing or even intense; it might involve shaking, crying, or feeling waves of heat as the body completes thwarted survival responses. While the outcome is a deeper, more resilient calm, the process itself is one of processing and completing, not just quieting. In therapy, we ensure this active release happens within a safe container, so it feels productive and integrating, not overwhelming.
Your Path to Embodied Healing: A Conclusion
Learning how to physically release trauma from the body is a courageous and transformative journey from fragmentation to wholeness. We've explored how trauma is not merely a story of the past but a living, breathing reality held within the body's nervous system and tissues. The chronic pain, tension, anxiety, and exhaustion you may be experiencing are not signs that you are broken; they are intelligent signals from a body that is still working to protect you from a danger that has long since passed.
The path to healing, therefore, lies not in ignoring these signals, but in learning to listen to them with compassion and skill. This article has outlined the key principles of this journey:
- Understanding the Physiology: Recognizing that trauma creates a dysregulated nervous system stuck in survival mode is the first step.
- Listening to the Body: Your physical symptoms are messengers, guiding you toward the areas that need healing and release.
- Utilizing Body-Based Therapies: Modalities like Attachment-Focused EMDR work directly with the brain and body's information processing system to integrate stuck memories and release their physical and emotional charge.
- Cultivating Safety: Gentle, consistent practices like grounding and paced breathing create the internal safety necessary for the nervous system to let go of its protective bracing.
- The Necessity of Guidance: A skilled trauma therapist provides a safe container, co-regulates your nervous system, and guides you through the process at a pace that feels manageable, preventing re-traumatization.
Releasing stored trauma is more than just symptom relief; it is a reclamation of your life force. As chronic tension melts away, you create space for more energy, deeper rest, emotional resilience, and a renewed sense of presence and joy. This journey is about creating the conditions for your nervous system to finally return to its natural state of balance, calm, and connection.
If you are an adult in New York ready to move beyond simply talking about your past and are seeking to do the deeper healing work that creates lasting change, I am here to guide you. My solo practice specializes in personalized, attachment-focused EMDR and EMDR Intensives designed to gently and effectively support the physical and emotional release of trauma. You do not have to walk this path alone.